Itching can sometimes appear out of nowhere, leading you to wonder where this mysterious itching came from. If the itching persists for longer than a couple of weeks, it might indicate that it’s caused by an underlying medical condition and would require a visit to your GP for a check-up. Read on for an overview of common itch triggers and tips for treatment below!
Reading time: 5.5 minutes
Common Symptoms
To help understand itching, it’s important to understand the basics of your body’s response. While often uncomfortable, an itch sensation is caused by irritation of skin cells or nerve cells associated with skin and is important for the body's self-protective mechanism.
Itching, otherwise known as pruritus , can occur in one part or all over of the body. It can also be accompanied by other symptoms including:
- Redness
- Rash
- Blisters
- Patches of irritated skin
- Scaly & dry skin
- Bumps & spots
While some symptoms are common with a specific factor, most of the time it’s quite difficult to identify where the new itch came from. You might benefit from reviewing the common factors below in order to help identify any potential changes in your life/routine that could have contributed to the sudden itch.

Itch triggers
Dehydrated/dry skin
- Commonly caused by lack of water or lack of natural oils, producing symptoms like scaly or flaky patches, redness and general irritation.
- While dry skin is sometimes a symptom for medical-related diseases, in most cases it’s fairly easy to treat by adding hydration and avoiding any factors that dehydrate your skin.
DO: Drink plenty of water and use an emollient body moisturizer after bathing
DON’T: Stay in hot water for a prolonged amount of time when bathing and avoid hygiene products with harsh chemicals & alcohols.

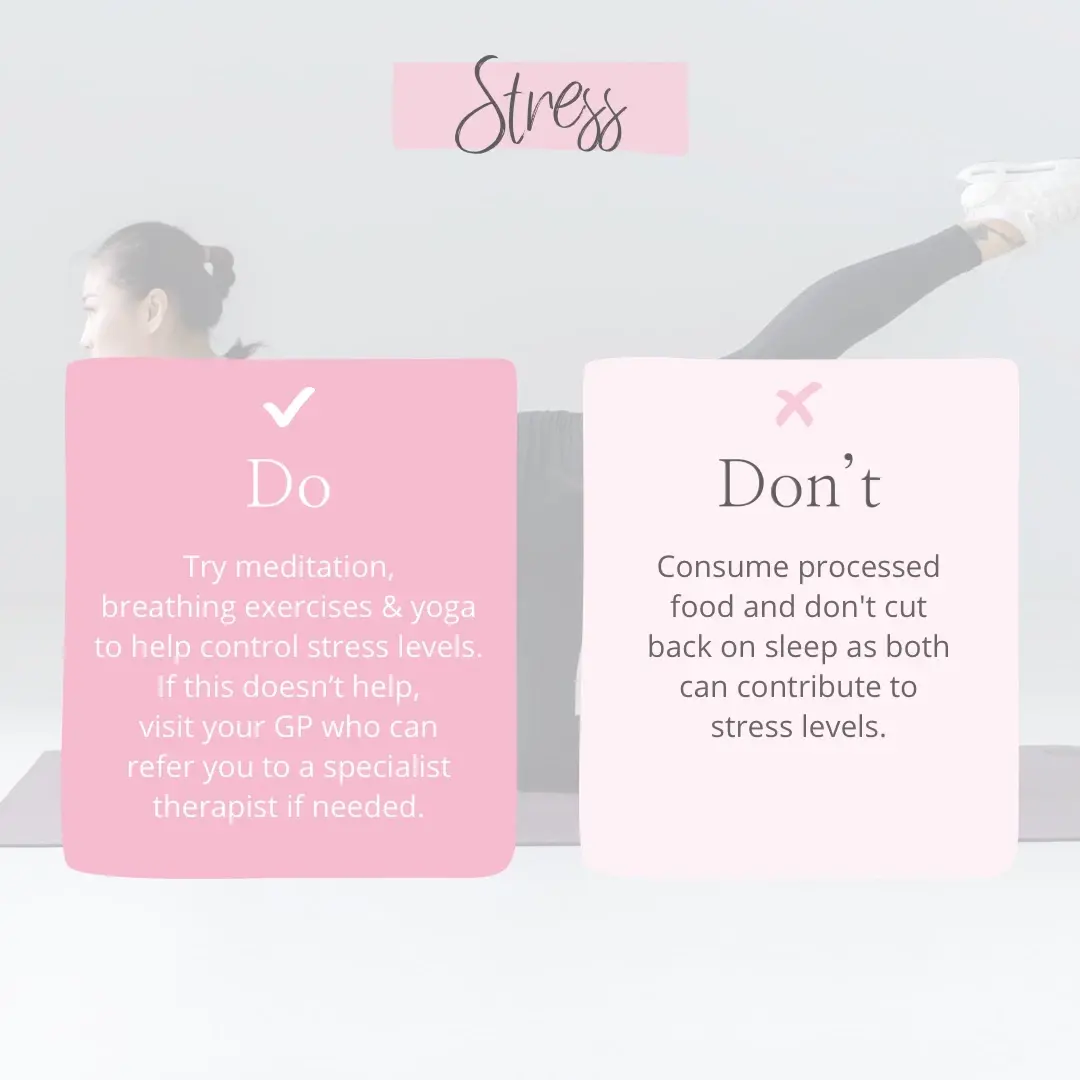
Stress
- Excessive stress can cause your body’s stress response to go into overdrive.
- This causes the brain to send sensory signals like itching to nerve endings in the skin.
DO: Try meditation, breathing exercises & yoga to help control stress levels. If this doesn’t help, visit your GP who can refer you to a specialist therapist if needed.
DON’T: Eat processed food and cut back on sleep as both can contribute to stress levels
Wool clothing
- While there has been some controversy about whether wool is actually an allergen.
- Recent data has found that a particular component of lanolin within might be causing the discomfort many associate with wearing wool, especially children.
DO: Avoid wearing wool if you can or wearing thick underlayers in order to reduce the contact with the skin.
DON’T: If you found that this irritates you, don’t use moisturisers and cosmetics containing lanolin.

Sleep deprivation
- Some deprive themselves of sleeping due to busy schedules, which can cause increased inflammation and stress, which are both linked to dry skin and itching.
- Others experience night time itching, otherwise known as nighttime pruritus, which tends to disturb sleep. For most people this is caused by the body's natural processes, which influence skin functions at night.
DO: Schedule in 7-9 hours of sleep a night to properly rest. If the itching is caused by nighttime pruritus, consider taking an antihistamine before bedtime or using an over-the-counter medicine that can help relieve the itch, like Eurax 10% Cream.
DON’T: Wear anything itchy for sleeping in and ensure that you don’t overheat the room prior to going to sleep as that can cause the air to dry out, furtherly drying out the skin.

Shower routine
- Showering/bathing for a prolonged period of time and using hot water can strip away natural oils from your skin, leaving your skin dry and itchy.
- Body washes and hygiene products containing alcohol, fragrance, dyes or antibacterial ingredients often irritate the skin, increasing the likelihood of itching and dryness of your skin.
DO: Opt for soap and hygiene product formulas that feature ‘for sensitive skin’, ‘hypoallergenic’, ‘moisturising’ claims.
DON’T: Keep the shower door open as it releases all the extra humidity produced by steam, which helps with the skin moisture levels.

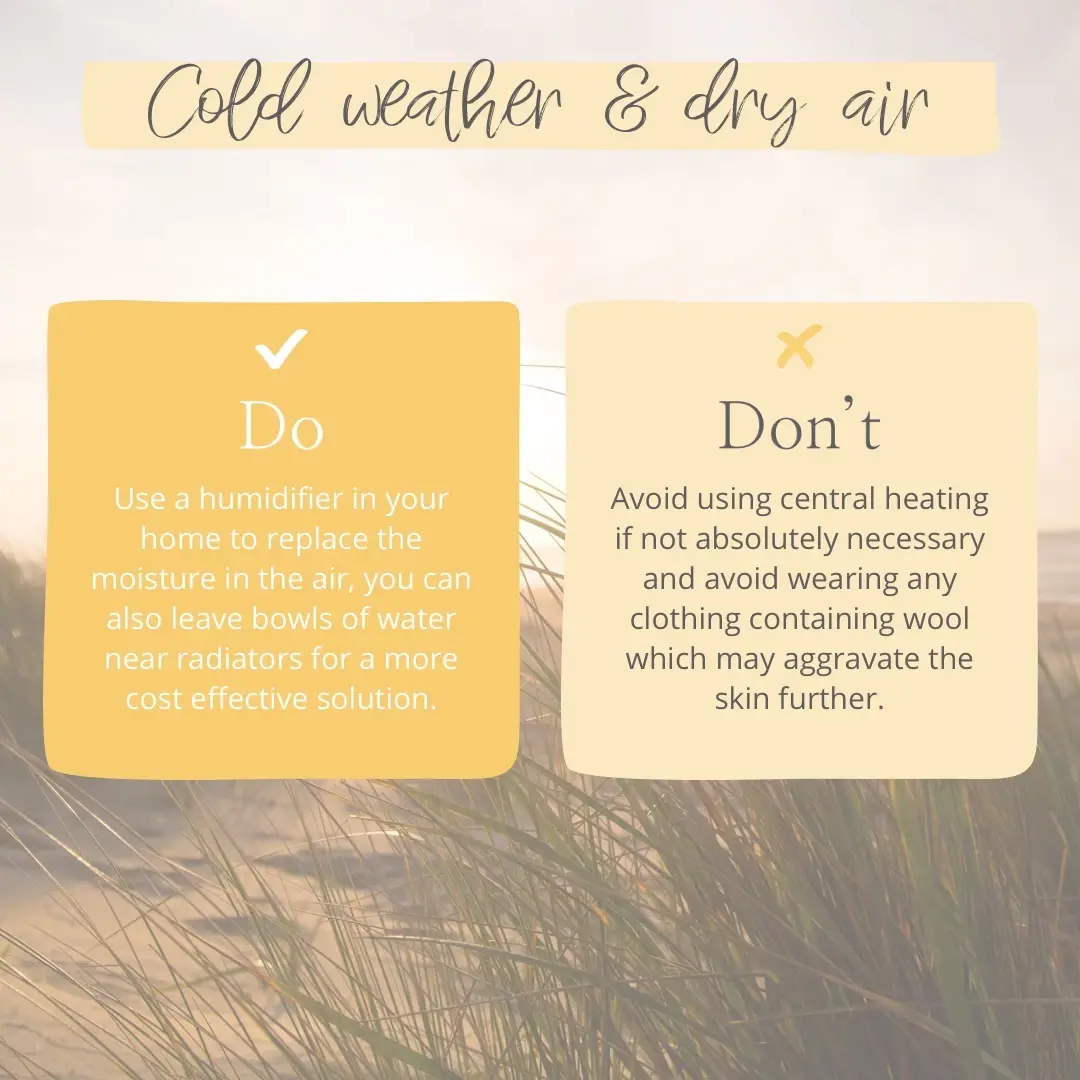
Cold weather & dry air
- Winter weather is often linked to dry skin during the colder months, however the exact cause of winter itch is unknown.
- Increased use of indoor heating is common in winter. Cold air that gets heated can cause air to dry out, and in turn, dry out skin by evaporating moisture from it.
DO: Use a humidifier in your home to replace the moisture in the air, you can also leave bowls of water near radiators for a more cost-effective solution.
DON’T: Avoid using central heating if not absolutely necessary and avoid wearing any clothing containing wool which may aggravate the skin further.
Hives/welts/nettle rashes
- Hives present as a raised and itchy skin rash, that is also often accompanied by redness of the affected area. They can appear in different shapes and sizes, however often cause itching or burning.
- They are not contagious as they’re most commonly caused by a reaction to an allergen, usually settling down within a few days.
DO: Take antihistamine if you don’t have any long-term conditions that might not allow you to use it. You can also use over-the-counter treatment options which can relieve itching and irritation caused by hives & nettle rashes, such as Eurax 10% Cream.
DON’T: Scratch the affected area as that could put you at risk of infection.

Insect bites
- Insect bites and stings often cause a red and itchy bump to appear in the affected area, however the symptoms will vary depending on which insect you were bitten by.
- Commonly associated with itching, mosquito bites cause saliva to enter the skin, which contains the protein that causes the allergic reaction due to the immune system response.
DO: Remove the sting if needed, take paracetamol or ibuprofen for the pain and consider applying a hydrocortisone cream to bites if itching is experienced.
DON’T: Scratch the bites as this can lead to damage of the skin and infection and avoid traditional home remedies as they’re unlikely to have an effect.

Heat rash/prickly heat
- Heat rash can appear anywhere on the body and usually presents as mildly swollen red spots on skin. This is often accompanied by an itchy, prickly feeling, which is why it’s also known as prickly heat.
- It is most commonly caused by skin overheating and is not contagious.
DO: Apply a cold compress to cool down the skin, wear loose clothing and spend as much time in air-conditioned spaces as possible. You may also use an ointment to help relieve discomfort in the affected areas.
DON’T: Bathe in hot water or use perfumed shower gels as they are likely to further aggravate your skin.

Medical causes
If you’ve tried to eliminate any likely environmental and lifestyle factors and haven’t noticed any improvement in reduction of itching, it might indicate that the itching is being caused by an underlying medical condition, however this is rare.
Some of the common conditions often linked to itching are:
- Eczema/dermatitis
- Psoriasis
- Scabies
- Chickenpox
- Anxiety/depression
- Diabetes
- Liver disease
- Anemia
- Thyroid problems
- Certain cancers
- Nerve disorders

When to see a GP/dermatologist
If the itching persists for longer than a couple of weeks, visit a GP for a consultation in order to determine the cause of the itch.
Some of the symptoms indicating a need of medical assistance include:
- Lasts longer than 2 weeks or keeps reoccurring
- Caused by a new rash or lump that you’re worried about
- Rash across the whole body
- Itching is affecting your daily life
Depending on what is determined during the assessment or if itching persists, you might be referred to a specialist for further evaluation, such as a dermatologist or an internist.